Leptospirosis is a zoonotic disease (infections that are spread between humans and animals) with epidemic potential caused by a bacterium called Leptospira. Leptospirosis occurs worldwide but is endemic mainly in countries with humid subtropical and tropical climates. A warm and humid environment promotes the survival of Leptospires. In the future, due to global warming and climate change problems, the disease may pose significant risks for other countries, including Türkiye.
The prevalence of Leptospirosis increases with natural disasters like floods, heavy and sudden rains, cyclones, tsunamis, land sliding and earthquakes.

The number of human cases is not known precisely due to under- or misdiagnosis. Still, it is estimated that there are more than 1,000,000 cases of Leptospirosis each year with about 59,000 deaths worldwide. In the Philippines and Peru, where Leptospirosis is a prominent threat, cases increased up to 70% and 188% accordingly in 2023, compared to the same period in 2022.
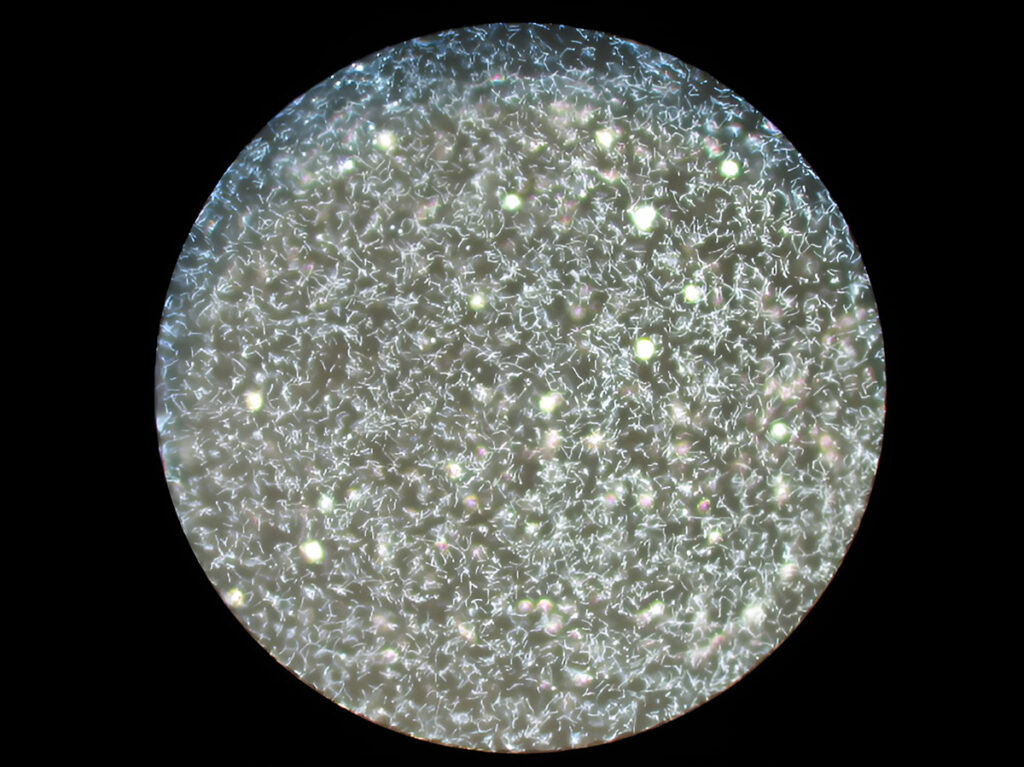
Leptospira is pathogenic to humans and animals with more than 200 serologic variants (distinct variations within a species). Humans can be infected with Leptospirosis through direct contact with the urine or other body fluids of the infected animals like cattle, pigs, horses, rodents, and dogs or urine-contaminated water, soil, or food. Human-to-human transmission is very rare.
Infected carrier animals could potentially remain symptom-free while shedding Leptospires for an entire lifetime.
Symptoms of Leptospirosis
Clinical manifestations of Leptospirosis may vary greatly from mild illness to serious even fatal disease. The time between a person’s exposure to Leptospira and becoming sick is 2 days to 4 weeks.
Leptospirosis usually presents four broad clinical categories:
- A mild, influenza-like illness
- Weil’s syndrome characterized by jaundice, renal failure, haemorrhage, and myocarditis with arrhythmias
- Meningitis/ Meningoencephalitis (inflammation of the protective membranes covering the brain and spinal cord/ additionally inflammation of the brain)
- Pulmonary haemorrhage with respiratory failure
The most common clinical features of Leptospirosis are fever, headache, chills, vomiting, myalgia (muscle aches and pain) especially in the calf muscle, jaundice (yellow skin and eyes), abdominal pain, diarrhoea, and conjunctival suffusion. This illness usually begins abruptly with fever and can last from 3 weeks or longer, and if not treated, even for several months.

Though, in some infected people, no symptoms can be observed, many of the reported cases have severe manifestations, for which mortality is greater than 10%.
Modes of Transmisison of Leptospirosis
The bacteria can enter the body through the skin especially if it is broken from a cut or scratch or mucous membranes of the eye, nose, and mouth. If you are in an area with Leptospirosis risk, you should avoid being exposed to possible contaminated water, soil and any infected animal or their urine. Protective clothing and sterilization with soap or alcohol is also advisable. Authorities warn against water sports, especially in high-risk tropical countries. Rodent prevention measures in these countries are also an important topic.
Risk Groups of Leptospirosis
The risk group for Leptospirosis are people who work outdoors or with animals like field workers, veterinarians, dairy workers, and military personnel.
This disease might also be a risk factor for your pet. Although clinical signs of Leptospirosis vary and are nonspecific, if you have suspicions, protect yourself from any possible contamination and urgently consult a veterinarian.
Treatment and Protection From Leptospirosis
Leptospirosis is treated with antibiotics such as doxycycline and penicillin, and even intravenous antibiotics may be required in severe cases.

The exact pathogenesis is still under research and although there are exciting new findings on this matter, there is still no vaccination for humans that protects against this disease. Vaccines have been developed for livestock animals, but they only protect against specific variants of Leptospira, and protection diminishes after one year.
Leptospirosis might be easily confused with other diseases like influenza, Dengue Fever, and viral haemorrhagic diseases since they share many symptoms. Therefore, to prevent outbreaks and save lives making an accurate diagnosis at the earlier onset of symptoms is very important for this disease. Real-Time PCR kits like Bosphore Tropical Fever Panel kit v1 from Anatolia, provide easy and accurate detection with high precision.
Bosphore Tropical Fever Panel Kit v1 also detects other common tropical pathogens like Plasmodium falciparum, Plasmodium malariae, Salmonella enterica, Plasmodium vivax, Dengue virus, Chikungunya virus, West Nile virus, and Plasmodium ovale, making the kit very efficient tool for both differentiating possible tropical diseases and making an early diagnosis.